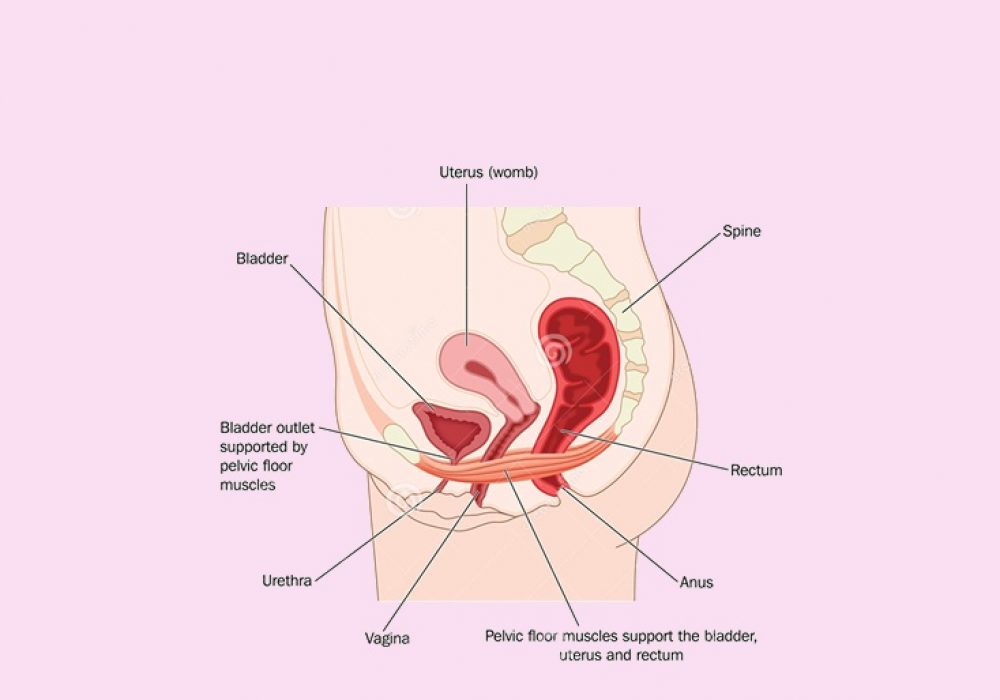
Mild uterine prolapses that cause no symptoms may not need treatment. For more serious prolapses, we will discuss both surgical and non-surgical options.
Non-Surgical Treatment for Uterine Prolapse Non-surgical options includethe insertion of a pessary which is a removable device that is inserted into the vagina to support the prolapsing muscles and organs.
Types of pessaries:
- Inflatable
- Doughnut
- Gellhorn
Your London Obs & Gynae consultant will recommend the correct type of pessary for you and can insert it whilst you are at our Clinic.
Your doctor may also recommend Kegel exercises. These are exercises designed to strengthen your pelvic floor muscles and can be performed easily anywhere – at home, while watching TV, in the car, or even at the office.
Lastly, women who are overweight or obese might find relief from their symptoms if they lose some excess weight. Weight loss can reduce pressure in the pelvis and relieve strain on their pelvic muscles.